Supporting Someone With PTSD PLR Course 23k Words
in Mental Health PLR , Mental Health PLR Ebooks , PLR eBooks , PLR eCourses , PLR List Building Reports , Premium PLR , Premium PLR eBooks , Premium PLR Reports , Premium White Label Brandable PLR Coaching Courses , Private Label Rights Products , Self Help PLR , Self Help PLR eBooks , Self Improvement PLR , Self Improvement PLR EbooksChoose Your Desired Option(s)
has been added to your cart!
have been added to your cart!
#ptsdsupport #mentalhealthawareness #supportstrategies #mentalhealthplr #plrcourse #mentalwellbeing #traumarecovery #emotionalsupport #selfhelpcontent #plrcontent
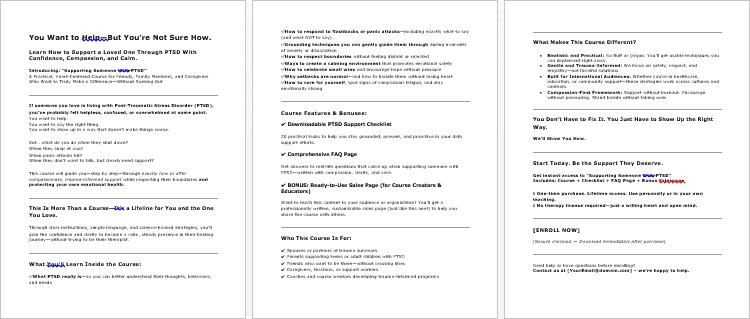
Supporting Someone With PTSD PLR Course: Empower Yourself to Be a Lifeline
Do you want to support someone living with PTSD but feel unsure where to start? Do you wish you had the knowledge and skills to make a real difference? The Supporting Someone with PTSD PLR Course is your solution. This comprehensive course is designed to give you the tools, strategies, and understanding needed to provide effective support with empathy and confidence.
Whether you’re a caregiver, friend, family member, or therapist, this step-by-step course will help you offer compassionate and informed support to someone living with PTSD. You’ll learn everything from recognizing symptoms to practicing self-care, so you can help others without burning out.
Presenting…
Supporting Someone With PTSD PLR Course 23k Words
Course Overview: Supporting Someone With PTSD
Supporting someone with PTSD can feel overwhelming, but with the right tools, it becomes manageable and even deeply rewarding. This 21,231-word course is structured into five insightful modules, each designed to guide you in providing holistic and mindful support to your loved ones, all while ensuring that you take care of your own mental and emotional health.
Module 1: Understanding PTSD – What It Really Means
To offer meaningful support, it’s crucial to understand PTSD, its causes, and how it manifests in daily life.
- Step 1: Learn What PTSD Is (And What It Isn’t)
Gain a clear understanding of PTSD, its psychological and physiological effects, and why it’s different from regular stress or anxiety. - Step 2: Recognize Common Signs and Symptoms
Identify emotional, behavioral, and physical symptoms like flashbacks, avoidance, and anxiety so you can spot them early and offer the best support. - Step 3: Understand PTSD Triggers
Learn how specific triggers—sights, sounds, smells, or events—can lead to PTSD episodes, and why these reactions are beyond the person’s control. - Step 4: Know the Types of Trauma
Explore the different types of trauma that can cause PTSD—such as abuse, accidents, and combat—and how each type affects the individual differently.
Module 2: Building a Foundation of Support
In this module, we’ll help you build a strong foundation to support your loved one in their healing journey.
- Step 1: Practice Empathetic Listening
Learn the art of listening without judgment, pressure, or fixing. Just being present can make all the difference. - Step 2: Use Calming Communication Techniques
Discover how to use tone, body language, and careful word choices to create a safe space for open, supportive conversations. - Step 3: Respect Their Boundaries
Learn the importance of respecting emotional and physical boundaries. Understand how to offer support without overwhelming or pushing too hard. - Step 4: Help Them Feel Safe
Discover how to create a stress-free environment and identify ways to help your loved one feel more secure and less anxious.
Module 3: Navigating Tough Times Together
Supporting someone through flashbacks, panic attacks, and crises requires specific techniques and strategies.
- Step 1: Support Through Flashbacks or Panic Attacks
Understand what to do—and what not to do—when your loved one experiences a flashback or panic attack. Learn how to handle these tough situations with care. - Step 2: Learn Grounding Techniques
Explore grounding exercises like the 5-4-3-2-1 method, which you can guide them through to help manage anxiety and panic. - Step 3: Know When to Step Back
Sometimes, giving space is the best way to support. Learn how to recognize when to step back and allow them to self-soothe. - Step 4: Have a Safety Plan in Place
Develop a gentle safety plan together in case of severe PTSD episodes, ensuring that both of you know what to do in a crisis situation.
Module 4: Encouraging Healing and Growth
Healing from PTSD is a journey, but you can encourage positive progress every step of the way.
- Step 1: Support Their Therapy or Treatment
Understand common therapies for PTSD like Cognitive Behavioral Therapy (CBT) and EMDR, and learn how to support them through their treatment journey. - Step 2: Help Rebuild Daily Routines
Explore ways you can help them structure their day—whether it’s meal times, sleep routines, or hobbies—promoting stability and healing. - Step 3: Celebrate Small Wins
Recovery is about celebrating every victory. Learn how to recognize and celebrate the small milestones that lead to big progress. - Step 4: Stay Patient Through Setbacks
Healing isn’t linear. This step will guide you on how to stay calm and supportive through challenging times and setbacks.
Module 5: Taking Care of You as a Supporter
You can’t help others effectively if you’re not taking care of yourself. This module helps you stay emotionally balanced.
- Step 1: Understand Compassion Fatigue
Supporting someone with PTSD can be emotionally draining. Learn to recognize the signs of compassion fatigue and how to manage your emotions. - Step 2: Set Healthy Boundaries for Yourself
Healthy support involves self-care. This step teaches you how to create personal boundaries to ensure that your emotional and physical needs are met. - Step 3: Find Your Own Support System
You’re not alone in this journey. Learn how to access support groups, local organizations, or online communities for caregivers and supporters. - Step 4: Practice Regular Self-Care
Self-care is vital for your well-being. Discover relaxation techniques and activities to recharge so you can continue supporting your loved one.
Additional Materials to Help You Succeed
To help you implement the lessons from the course and provide even more value to your customers, this PLR package includes:
- Supporting Someone With PTSD – Checklist (577 words): A quick reference guide to help you implement the strategies learned in the course.
- Supporting Someone With PTSD – FAQs (759 words): A comprehensive FAQ that answers common questions about PTSD and how to support a loved one.
- Supporting Someone With PTSD – Sales Page (602 words): A professionally crafted sales page to help you effectively market the course.
How to Profit from the Supporting Someone With PTSD Course
This Supporting Someone With PTSD PLR Course provides a fantastic opportunity for multiple streams of income. Here are several ways you can use this course to build your business:
- Sell the Course as-is: Offer the complete course directly on your website for $47-$97 depending on your market.
- Break the Course Into Modules: Turn the course into smaller, bite-sized reports or mini-courses and sell each one for $10-$20.
- Bundle with Related Products: Combine this course with other wellness or mental health products and sell the bundle for $97-$197.
- Create a Membership Site: Set up a membership site where customers pay a monthly fee for access to the course and additional resources, creating passive income.
- Offer Coaching Services: Add one-on-one coaching or group coaching for people supporting someone with PTSD as an upsell.
- Convert to Audio/Video: Create an audio or video version of the course and sell it for $297-$497 for a more premium offering.
What You Can Do with This Course:
Permissions:
- Sell the course as-is or with minor tweaks to make it your own.
- Break the content into small reports and sell them individually for $10-$20 each.
- Bundle the course with other related products and sell it for $97–$197.
- Create a membership site and charge recurring fees.
- Convert the content into audio or video formats and sell for a premium price.
- Use portions of the content for lead magnets to grow your email list.
Restrictions:
- You cannot pass on PLR rights to your customers.
- You cannot offer 100% affiliate commissions.
- The full course cannot be given away for free in its current state—it must be sold or excerpted/modified for giveaways.
Support Someone with PTSD—Become a Lifeline Today
Empower yourself with the knowledge and skills to support someone living with PTSD. With the Supporting Someone With PTSD PLR Course, you can provide compassionate, informed care while maintaining your own emotional balance.
Get started today and help make a positive difference in someone’s life. Start your journey toward becoming a PTSD supporter now!
has been added to your cart!
have been added to your cart!
Here A Sample of Supporting Someone With PTSD PLR Course
Helping someone with PTSD can feel overwhelming—but with the right understanding, empathy, and strategies, you can make a big difference in their life. This course is designed to guide you step-by-step through the essential knowledge and skills needed to support someone living with PTSD with compassion and confidence.
Module 1: Understanding PTSD – What It Really Means
Step 1: Learn What PTSD Is (And What It Isn’t)
Welcome to Step 1: Gaining a Clear Understanding of PTSD
Before we dive into how to support someone with PTSD, it’s crucial that you first understand exactly what PTSD is—and what it is not. In this step, we’ll explore the foundational knowledge of Post-Traumatic Stress Disorder (PTSD) from an international perspective, looking at how it develops, how it affects the brain and body, and how it differs from normal stress or anxiety. This knowledge will help you support others from a place of clarity, empathy, and confidence.
1. What Is PTSD?
PTSD stands for Post-Traumatic Stress Disorder, a mental health condition that can develop after a person experiences or witnesses a traumatic event. The event might involve actual or threatened death, serious injury, or sexual violence—either directly, by witnessing it, or by learning it happened to someone close.
According to the World Health Organization (WHO) and the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), PTSD is diagnosed when symptoms persist for more than one month and interfere with a person’s daily life.
Common examples of traumatic events include:
- Military combat
- Natural disasters (earthquakes, floods, fires)
- Serious accidents (car crashes, workplace injuries)
- Physical or sexual assault
- Childhood abuse or neglect
- Terrorist attacks or war experiences
It’s important to remember that trauma is subjective—what one person finds traumatic, another may not. PTSD is not about “toughness” or “mental strength”; it is a neurobiological response to overwhelming stress.
2. What Happens in the Brain and Body During PTSD?
PTSD affects the brain’s survival system, especially the following areas:
- Amygdala (alarm system): Becomes overactive, leading to heightened fear responses.
- Hippocampus (memory center): May shrink or malfunction, causing confusion between past and present threats (e.g., flashbacks).
- Prefrontal cortex (logic and reasoning): May become underactive, reducing the brain’s ability to calm the amygdala or logically assess danger.
This brain imbalance leads to ongoing fight, flight, or freeze responses, even when no real threat is present. The body stays on high alert, flooding with stress hormones like cortisol and adrenaline, which can lead to physical symptoms such as:
- Rapid heart rate
- Shallow breathing
- Sleep disturbances
- Muscle tension
- Gastrointestinal problems
PTSD is not just psychological—it’s deeply biological and neurological, which is why simply “thinking positively” or “snapping out of it” doesn’t work.
3. PTSD vs. Everyday Stress or Anxiety: What’s the Difference?
One of the biggest misconceptions is confusing PTSD with normal stress or even generalized anxiety disorder (GAD). Let’s clarify the differences:
| Feature | PTSD | Everyday Stress / GAD |
| Cause | Linked to a specific traumatic event | May be situational or general |
| Duration | Chronic, can last months or years | Often short-term or tied to specific issues |
| Symptoms | Flashbacks, nightmares, hypervigilance | Worry, restlessness, muscle tension |
| Triggers | Often specific to the trauma | Often vague or generalized |
| Impact | Major disruption to life and function | May cause discomfort but not always disabling |
| Body Response | Constant state of high alert (fight/flight) | Intermittent anxiety, but calmer baseline |
PTSD is a disorder, not just a feeling. It often shows up even when a person wants to feel normal or “move on.” It is not a weakness—it’s a normal response to an abnormal event.
4. Cultural and Global Considerations
PTSD affects people worldwide, regardless of culture, language, or geography. However, the way trauma is expressed and treated may vary:
- In Western countries, PTSD may be diagnosed and treated with psychotherapy and medication.
- In non-Western or collectivist societies, trauma may be expressed more through physical symptoms (like headaches or fatigue), or through spiritual beliefs.
- Stigma around mental illness can also prevent individuals from seeking help, especially in communities where expressing emotion is discouraged or mental health care is limited.
As a supporter, it’s essential to approach PTSD with cultural sensitivity. Be open-minded and non-judgmental. Understand that healing may look different depending on the person’s cultural background and available support systems.
5. Key Takeaways for This Step
- PTSD is a mental health condition caused by trauma, not by weakness or personality flaws.
- It involves real brain and body changes that affect memory, emotion, and physical wellbeing.
- PTSD is not the same as stress or anxiety. It’s more intense, long-lasting, and connected to a specific trauma.
- Symptoms may include flashbacks, nightmares, hypervigilance, avoidance behaviors, and strong emotional reactions.
- Cultural and international context matters—approach with awareness and sensitivity.
Self-Reflection Question (Optional Activity):
Take a few moments to reflect or journal on the following:
Have you ever misunderstood someone’s behavior because you didn’t know they were dealing with trauma or PTSD? How might understanding what you’ve learned today help you approach things differently?
This step is about building your foundation. As we move forward in the course, you’ll be able to apply this understanding in practical ways that help someone feel seen, safe, and supported.
Step 2: Recognize Common Signs and Symptoms
Welcome to Step 2: Identifying the Signs of PTSD
Now that you understand what PTSD is and how it differs from regular stress, it’s time to get specific. In this step, we’ll explore how PTSD shows up in real life—emotionally, behaviorally, and physically. These symptoms often appear gradually and can be easily misunderstood or dismissed, so learning to recognize them is key if you’re going to provide meaningful support.
Understanding these symptoms will help you notice red flags early, respond with empathy, and avoid misjudging someone’s reactions. This step is particularly useful for trainers, caregivers, educators, community workers, and anyone supporting individuals across different cultural or global backgrounds.
1. Emotional Symptoms of PTSD
Emotional responses are often the most noticeable signs of PTSD—though they may not always be obvious to an outsider. Trauma survivors may struggle with overwhelming emotions or a lack of emotion altogether, depending on how they process their experiences.
Key emotional symptoms to look for:
- Intrusive thoughts: Constant, unwanted memories of the traumatic event that feel inescapable.
- Flashbacks: The individual relives the trauma in vivid detail, as though it’s happening all over again. This can include intense fear, physical reactions, or dissociation.
- Nightmares: Repeated distressing dreams that may replay the trauma or include related fear themes.
- Mood swings: Unpredictable shifts between anger, sadness, fear, guilt, or numbness.
- Emotional numbness or detachment: A person may seem emotionally shut down, distant, or disconnected from loved ones or activities they once enjoyed.
- Guilt or shame: This is especially common in survivors of interpersonal trauma (e.g., abuse, assault, war). They may feel responsible for what happened.
These emotional responses are not signs of “drama” or “overreaction.” They are survival responses—the mind trying to make sense of or defend against danger that it hasn’t processed yet.
2. Behavioral Symptoms of PTSD
Behavior changes are often misunderstood, especially in workplace, school, or family settings. People may think the person is being moody, defiant, lazy, or antisocial—but often, these behaviors are coping mechanisms.
Common behavioral signs include:
- Avoidance: Steering clear of anything that reminds them of the trauma—this could be places, people, conversations, or even specific smells or sounds.
- Isolation or withdrawal: Choosing to be alone, not returning calls or messages, or pulling away from social events.
- Hypervigilance: Constantly being on alert or “on edge,” scanning the environment for threats even when it seems safe.
- Irritability or aggression: Sudden outbursts of anger or frustration, often over small triggers.
- Substance use: Alcohol, drugs, or even excessive medication use to self-soothe or escape intrusive thoughts.
- Difficulty concentrating: Trouble focusing on tasks or following conversations, especially in noisy or unpredictable environments.
People with PTSD aren’t trying to be difficult—they are adapting to a perceived threat. Their behaviors are protective, even if they seem puzzling or disruptive to outsiders.
3. Physical Symptoms of PTSD
Many trauma survivors experience very real, very persistent physical symptoms, which often go unrecognized as being linked to PTSD. These symptoms may even result in frequent medical visits or tests, especially in countries or communities where mental health is stigmatized or poorly understood.
Physical symptoms may include:
- Fatigue: Constant tiredness, even with adequate rest, due to hyperarousal and emotional overload.
- Headaches: Tension headaches or migraines from chronic stress.
- Digestive issues: Nausea, stomach pain, IBS-like symptoms, or changes in appetite.
- Sleep problems: Trouble falling asleep, staying asleep, or experiencing non-restorative sleep due to nightmares or anxiety.
- Startle response: Jumping easily at sudden noises or unexpected touch.
- Muscle tension or body pain: Especially in the neck, shoulders, and back, due to being in a heightened state of alertness.
These symptoms may mimic physical illnesses, but they are often rooted in chronic nervous system dysregulation—the body remaining in fight-or-flight mode even when there’s no immediate danger.
4. Cultural and Global Variations in Symptoms
PTSD symptoms don’t always look the same across cultures. In some parts of the world, emotional pain is expressed more through physical complaints or spiritual beliefs, due to social norms around emotional expression or the availability of mental health care.
For example:
- In some cultures, somatization is more common—where emotional distress is expressed as physical pain.
- A person might describe feeling cursed, haunted, or spiritually attacked rather than saying “I have trauma.”
- Children might show symptoms through behavioral regression (bedwetting, tantrums) or school refusal, rather than discussing fear or nightmares.
- Community-based healing or religious rituals might be preferred over therapy in many societies.
As someone supporting individuals across different regions, it’s essential to understand that trauma doesn’t always speak in the language of psychology. Be open to how symptoms are framed and expressed in the individual’s culture.
5. PTSD Symptoms at a Glance: An International Summary
| Symptom Type | Common Expressions |
| Emotional | Flashbacks, fear, guilt, numbness, irritability |
| Behavioral | Avoidance, aggression, social withdrawal, substance use |
| Physical | Sleep issues, fatigue, muscle tension, GI problems |
| Cultural Framing | Spiritual distress, physical complaints, family withdrawal |
Understanding these symptoms will help you avoid making assumptions. When someone is acting “difficult,” they may actually be acting “wounded.” When someone is quiet or withdrawn, they may not be unfriendly—they may be in survival mode.
Self-Check: Reflect on Your Awareness
Ask yourself:
“If someone close to me was experiencing these symptoms, would I recognize them as signs of trauma? Or would I misunderstand their behavior?”
As a supporter, your job isn’t to diagnose, but to observe and listen with awareness. Recognizing the symptoms is the first step in helping someone feel safe and understood.
This concludes Step 2: recognizing the common signs and symptoms of PTSD. By sharpening your awareness of how trauma shows up emotionally, behaviorally, and physically—and across cultures—you’re building the tools to become a sensitive, informed, and effective support person.
Step 3: Understand PTSD Triggers
Welcome to Step 3: Understanding PTSD Triggers
This step focuses on a critical element of post-traumatic stress: triggers. A trigger is any stimulus—external or internal—that reminds a person of a traumatic experience and causes them to react as if the danger were happening again, even when they are safe in the present.
In this step, you’ll learn what triggers are, how they work in the brain, common types of triggers, and most importantly, why they are not something a person can simply ignore or “get over.” Understanding this will help you become a more compassionate, patient, and prepared supporter.
1. What Are PTSD Triggers?
Triggers are sensory reminders of a past trauma that activate the brain’s survival system. The reminder can be obvious, like hearing fireworks that resemble gunfire, or subtle, like the smell of perfume worn by an abuser.
For someone with PTSD, encountering a trigger doesn’t just cause mild discomfort. It can hijack their nervous system, causing emotional distress, physical symptoms, or behaviors meant to protect them—even if there’s no actual threat in the present.
Here’s how it works in the brain:
- The amygdala, which processes fear, becomes hyperactive in people with PTSD.
- When a trigger is encountered, the amygdala sends a danger signal—even if there is no real danger.
- The prefrontal cortex (the logical, reasoning part of the brain) is overridden by this fear response.
- The body reacts with fight, flight, freeze, or fawn—often before the person can consciously process what is happening.
The reaction is automatic, physiological, and not a choice.
2. Common Types of Triggers
Triggers can vary widely from person to person based on their trauma history. For course participants or professionals working in diverse cultural or international contexts, it’s essential to realize that what may seem harmless to one person could be deeply distressing to another.
Let’s break this down into external and internal triggers.
A. External Triggers
These are cues from the outside world that resemble something from the traumatic event.
Examples:
- Sights: A person in a uniform, flashing lights, or a dark alley.
- Sounds: Loud bangs, shouting, sirens, or sudden music changes.
- Smells: Smoke, alcohol, antiseptic, or a specific type of food.
- Touch: Being unexpectedly touched, especially from behind.
- Places: Hospitals, basements, hotels, or any location linked to the trauma.
- Anniversaries or holidays: Certain dates or times of year can trigger painful memories.
B. Internal Triggers
These come from within the person and are harder to recognize, but just as powerful.
Examples:
- Emotions: Feeling helpless, lonely, or angry—emotions felt during the trauma.
- Physical sensations: A racing heartbeat, tight chest, or shortness of breath.
- Thoughts or memories: Unwanted mental images or flashbacks.
- Body posture or movement: Lying in a position similar to how they were during the trauma.
Important note: What triggers one person may not affect another at all. Triggers are highly individual, and many trauma survivors may not even be fully aware of all their triggers until they experience them.
3. Why Triggers Are Not Voluntary Reactions
One of the most harmful misconceptions about PTSD is that people should just “get over it” or “calm down” when triggered. This step is about correcting that narrative.
Here’s what supporters and course creators must remember:
- Triggers bypass rational thought. The trauma memory is stored in the brain’s emotional center, not in the logical part.
- The body reacts automatically. When triggered, the survivor may experience racing heart, sweating, trembling, or a feeling of being “out of body.”
- They’re not pretending. The fear, anger, or shut-down response is not exaggerated. To their brain, the threat feels real and immediate.
- “Snapping out of it” is not possible. Telling someone to relax or calm down during a trigger may make them feel unsafe or ashamed.
The most effective support is compassion, validation, and creating a sense of safety without pressuring the person to “move on.”
4. Practical Examples Across Cultures and Environments
Understanding triggers is essential for professionals working internationally. The same traumatic event may have different triggers depending on culture, environment, and context.
Consider these examples:
- A refugee from a war-torn country may be triggered by military helicopters or even loud celebratory fireworks, which might be normal in another culture.
- A survivor of domestic violence might be triggered by specific phrases or tones of voice, especially if they echo past verbal abuse.
- A natural disaster survivor could become anxious during thunderstorms, even if the danger is minimal.
- A child growing up in a violent neighborhood might feel panic at the sound of popping balloons.
- In some cultures, people may interpret their triggers as a spiritual or ancestral disturbance, rather than a psychological response—this needs to be respected, not dismissed.
For international course creators, trainers, or therapists, being aware of cultural framing is key. How trauma is experienced and how triggers are described varies significantly—and your language and response should reflect cultural sensitivity.
5. Supporting Someone During a Trigger: Do’s and Don’ts
If you’re in a position to support someone when they’re triggered, your response can make a huge difference in either de-escalating the fear response or making the person feel more isolated and unsafe.
Do:
- Stay calm. Your nervous system can help calm theirs.
- Speak gently and slowly. Use short, non-threatening sentences like, “You’re safe right now,” or “I’m here with you.”
- Ask what they need. If they’ve previously shared coping tools (like deep breathing, grounding), remind them.
- Give them space. Some people need to move or be alone to regulate.
Don’t:
- Touch without permission. Even if you mean well, physical contact may intensify the panic.
- Tell them to calm down or stop. This invalidates their experience.
- Minimize the reaction. Saying “it’s not a big deal” or “just relax” can damage trust.
- Force conversation. Let the person re-engage on their own terms.
Conclusion: Respect the Power of Triggers
Triggers are not signs of weakness. They are reminders of a time when a person’s safety, control, or dignity was taken from them. Your role isn’t to fix or erase these triggers—but to understand them, respect their power, and respond with empathy and education.
By recognizing how triggers show up and how trauma rewires the brain and body, you’re laying the groundwork for trauma-informed care and communication. Whether you’re a caregiver, educator, coach, or international course creator, this knowledge helps you build safer environments for everyone.
Step 4: Know the Types of Trauma
Welcome to Step 4: Know the Types of Trauma
In this final step of Module 1, we’ll broaden our perspective by looking at what kinds of life experiences can lead to PTSD and how these different types of trauma can affect people in varied and deeply personal ways. Too often, trauma is narrowly associated with war or physical assault, but the truth is: trauma wears many faces, and no one is immune to it.
Understanding the range of trauma types is critical for international course creators, caregivers, educators, and mental health supporters. Each form of trauma carries its own emotional weight, memory imprint, and set of possible triggers. This step helps you recognize the diversity of trauma origins, reduce stigma, and respond more empathetically to survivors, regardless of how their trauma occurred.
1. Defining Trauma and Its Impact
At its core, trauma is the emotional and psychological response to an event that overwhelms a person’s ability to cope.
Trauma is not defined solely by the event itself, but by the person’s subjective experience of it. Two people could go through the same experience and have different reactions—one may recover without lasting symptoms, while the other could develop PTSD.
Trauma becomes PTSD when the symptoms persist for more than a month and significantly impact a person’s functioning in daily life. Not all trauma leads to PTSD—but all trauma deserves to be taken seriously.
2. The Major Types of Trauma
Let’s look at the most common categories of trauma that can lead to PTSD. For each one, we’ll explore what it might involve, how it can affect someone’s mental and emotional state, and how it may present in behavior.
A. Acute Trauma
Definition:
This is trauma that results from a single distressing event, such as a serious accident or natural disaster.
Examples:
- Car crash
- Robbery or physical assault
- Sudden medical emergency
- House fire
- Earthquake or flood
Possible Responses:
- Flashbacks to the moment of the incident
- Hypervigilance in similar environments (e.g., driving, hospitals)
- Avoidance of reminders like roads, loud noises, or emergency sirens
International Note:
Acute trauma is often visible in the aftermath of humanitarian crises, climate disasters, or political unrest. Emergency responders and community leaders must understand how single events can shape mental health long-term.
B. Chronic Trauma
Definition:
This is trauma that occurs repeatedly and over an extended period. It often happens in environments where the person cannot escape the threat.
Examples:
- Domestic violence
- Long-term childhood abuse or neglect
- Bullying
- Living in a war zone
- Repeated exposure to violent crime
Possible Responses:
- Difficulty trusting others
- Trouble forming healthy relationships
- Feelings of helplessness or learned hopelessness
- Emotional numbness or shutdown
International Note:
In certain global contexts—such as communities facing systemic oppression or generational violence—chronic trauma may be normalized or underreported. Recognizing this pattern is essential for sensitive support.
C. Complex Trauma
Definition:
This refers to exposure to multiple traumatic events, often of an interpersonal nature, and typically starting in early life. It’s sometimes seen as a combination of acute and chronic trauma.
Examples:
- Childhood abuse combined with neglect
- Human trafficking
- Repeated sexual or emotional abuse by caregivers
- Abandonment in foster care or institutions
Possible Responses:
- Deep-rooted issues with identity and self-worth
- Severe emotional dysregulation
- Dissociation or difficulty staying grounded
- Suicidal thoughts or high-risk behaviors
International Note:
Complex trauma is particularly relevant when working with refugee populations, survivors of childhood institutions, or individuals from conflict zones where multiple traumas are layered over time. This group often needs long-term and trauma-informed care.
D. Secondary or Vicarious Trauma
Definition:
This is trauma experienced indirectly by witnessing or hearing about another person’s trauma—common among caregivers, first responders, therapists, or even media consumers.
Examples:
- Social workers hearing abuse disclosures
- Emergency doctors witnessing critical injuries daily
- Journalists covering war or violent crime
- Family members of trauma survivors
Possible Responses:
- Compassion fatigue or burnout
- Emotional numbing or withdrawal
- Anxiety and difficulty sleeping
- Guilt or helplessness
International Note:
In high-trauma regions, aid workers, teachers, and health professionals may experience vicarious trauma even if they’re not the direct victims. Training and support for these helpers is just as important as support for survivors.
E. Developmental Trauma
Definition:
This form of trauma stems from disruptions in early attachment relationships, usually during childhood.
Examples:
- Separation from caregivers
- Emotional neglect
- Exposure to caregiver addiction or mental illness
- Institutionalization without consistent attachment
Possible Responses:
- Difficulty regulating emotions and stress
- Trouble with authority or attachment figures
- Impaired sense of identity or self-safety
- High risk of re-traumatization in adulthood
International Note:
In regions with high orphan rates, economic migration, or conflict-related displacement, developmental trauma can be widespread. Early interventions and long-term relational support are key in these cases.
3. Grief and Loss: A Hidden Trauma
Loss of a loved one—whether through death, divorce, or estrangement—can be deeply traumatic, especially if sudden, violent, or unresolved. PTSD can develop when grief is complicated by traumatic circumstances, such as:
- Violent or accidental death
- Death during childbirth
- Disappearance (e.g., during war, kidnapping)
- Pandemic-related loss without closure
While not always labeled as trauma, grief can have similar symptoms, including:
- Intrusive memories of the person’s last moments
- Feelings of guilt, blame, or regret
- Avoidance of reminders
- Sleep disturbances and social withdrawal
This kind of trauma often goes unrecognized, but acknowledging it is vital for healing and support.
4. Cultural and Global Perspectives on Trauma
Trauma doesn’t exist in a vacuum—it’s shaped by cultural beliefs, social structures, and language. What one culture labels as trauma, another may interpret as fate, punishment, or spiritual imbalance.
When teaching, counseling, or supporting people from international backgrounds, remember:
- Language matters. Some cultures may not use the term “trauma” or may have no direct translation.
- Expression varies. In some cultures, trauma is expressed through physical symptoms (e.g., headaches, stomach pain), while others may focus on dreams or social withdrawal.
- Community plays a role. Some societies prioritize community healing over individual therapy.
- Stigma is real. Talking about mental health may be taboo, leading to silence or shame.
As an international course creator, your trauma education should be inclusive, respectful, and adaptable to varied belief systems and communication styles.
Conclusion: Understanding Trauma Is Foundational
Recognizing the different types of trauma is not about labeling people—it’s about creating deeper empathy. When you understand where a person’s trauma may have come from, you can better support their path forward.
Each survivor’s journey is unique. What one person carries from a single incident, another may carry from years of neglect. Your role is not to compare or judge—but to listen, learn, and provide support with informed compassion.
By understanding the origins of PTSD and the many faces of trauma, you’re now better prepared to approach support work with a wider lens and an open heart.
We’re also giving these extra bonuses
Supporting Someone With PTSD – Checklist
Supporting Someone With PTSD – FAQs
Supporting Someone With PTSD – Salespage Content
Package Details:
Word Count: 21 231 Words
Number of Pages: 105
Supporting Someone With PTSD – Bonus Content
Checklist
Word Count: 577 words
FAQs
Word Count: 759 words
Salespage Content
Word Count: 602 words
Total Word Count: 23 169 Words
Your PLR License Terms
PERMISSIONS: What Can You Do With These Materials?
Sell the content basically as it is (with some minor tweaks to make it “yours”).
If you are going to claim copyright to anything created with this content, then you must substantially change at 75% of the content to distinguish yourself from other licensees.
Break up the content into small portions to sell as individual reports for $10-$20 each.
Bundle the content with other existing content to create larger products for $47-$97 each.
Setup your own membership site with the content and generate monthly residual payments!
Take the content and convert it into a multiple-week “eclass” that you charge $297-$497 to access!
Use the content to create a “physical” product that you sell for premium prices!
Convert it to audios, videos, membership site content and more.
Excerpt and / or edit portions of the content to give away for free as blog posts, reports, etc. to use as lead magnets, incentives and more!
Create your own original product from it, set it up at a site and “flip” the site for megabucks!
RESTRICTIONS: What Can’t You Do With These Materials?
To protect the value of these products, you may not pass on the rights to your customers. This means that your customers may not have PLR rights or reprint / resell rights passed on to them.
You may not pass on any kind of licensing (PLR, reprint / resell, etc.) to ANY offer created from ANY PORTION OF this content that would allow additional people to sell or give away any portion of the content contained in this package.
You may not offer 100% commission to affiliates selling your version / copy of this product. The maximum affiliate commission you may pay out for offers created that include parts of this content is 75%.
You are not permitted to give the complete materials away in their current state for free – they must be sold. They must be excerpted and / or edited to be given away, unless otherwise noted. Example: You ARE permitted to excerpt portions of content for blog posts, lead magnets, etc.
You may not add this content to any part of an existing customer order that would not require them to make an additional purchase. (IE You cannot add it to a package, membership site, etc. that customers have ALREADY paid for.)
Share Now!